By Antonia Johnson, Brad R Johnson, MD, Jennifer White Johnson, MD, Laura Gonzalez-Krellwitz, MD, Patricia Connor, MD, Sandra Marchese Johnson, MD
Case Presentation
A 2-month-old fraternal twin female presented to the dermatologist with a firm red mass on the right lateral thigh (figure 1). The growth started at birth as a nickel-sized red patch and continued to grow. When presenting to us, our differential diagnosis included juvenile xanthogranuloma and histiocytoma. A 3mm punch biopsy was performed. The histology revealed a spindle cell 24 proliferation with fibrohistiocytic differentiation. While special stains were pending, the patient returned to the clinic twelve days later with rapid growth of the lesion and was referred to the local children’s hospital (figure 2). At the hospital, an MRI revealed a 3.5 x 2.2 x 3.8 cm tumor.
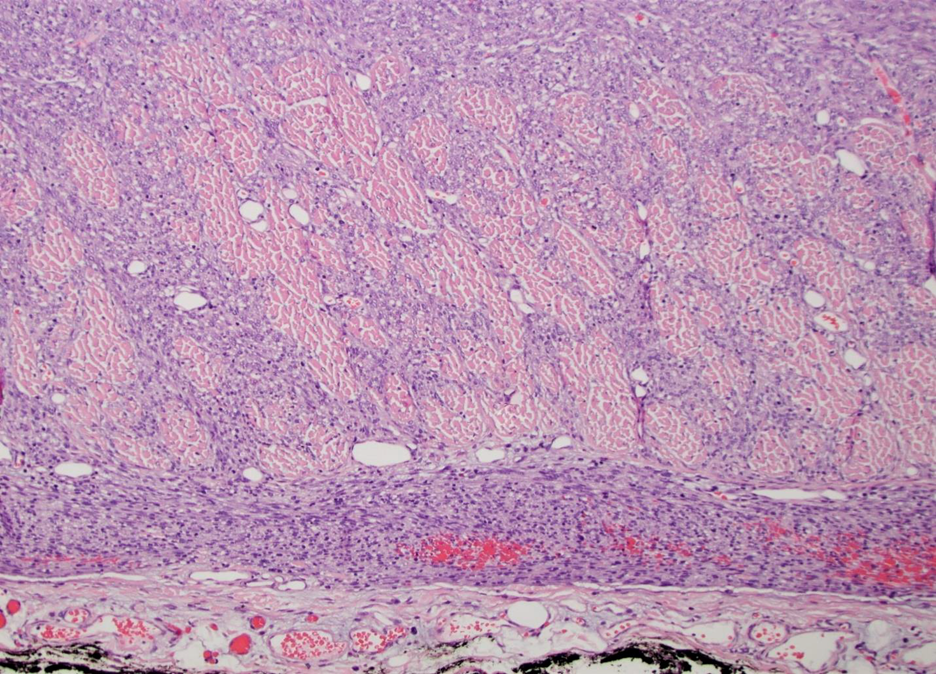
The growth was fully excised and sent directly to their pathology department. At this point, the tumor was identified as infantile fibrosarcoma based on the histology and special stains. There is invasion through the deep dermis and subcutaneous layers by oval to spindled neoplastic cells arranged in intersecting fascicles and herringbone patterns. Mitosis were common (figures 3,4,5).
Discussion
Infantile fibrosarcoma (IFS) is a rare tumor (5 cases of IFS per 1,000,000 babies1) accounting for about a quarter of all soft tissue sarcomas observed within one year of birth2. Approximately 80% of cases are diagnosed within the first year of life2. Less than half are diagnosed in utero or at the time of birth1. IFS is caused by an ETV6–NTRK3 translocation of genetic information causing children to develop malignant tumors originating in the soft tissue3. These rapidly growing tumors are usually present at the time of birth or appear very shortly thereafter and are 39 typically found on the arms or legs of the infants3.
The recommended treatment for infantile fibrosarcoma is non-mutilating surgery. If this is not possible due to the size of the tumor, placement, or other factors, chemotherapy with vincristine plus dactinomycin is recommended. This chemotherapy treatment seems to be the safest and least toxic treatment for children with IFS. Chemotherapy can also be used after surgery if most of the tumor is removed but the margins of the excision are not clear. If non-mutilating surgery and chemotherapy are not effective, mutilating surgery should be considered. Radiotherapy is to be used cautiously in these scenarios due to possible negative untoward effects3.
IFS has a heartening prognosis. Around 80% are potentially cured. The 10-year survival rate is about 90%. IFS does need long-term oncological care. However, the occurrence of a malignant tumor at this young age raises concern about future malignant tumors and possible metastases3. This particular patient is getting long-term care established at the local children’s hospital oncology center. She had non-mutilating surgery and is doing well at the time this case was submitted.
Figure 1: initial presentation with firm tumor on the lateral thigh

Figure 2: Rapid growth of tumor within 12 days

Figure 3. H&E 4x. Epidermal hyperplasia overlying a monomorphic cellular infiltrate expanding the dermis with entrapment of adnexal structures.
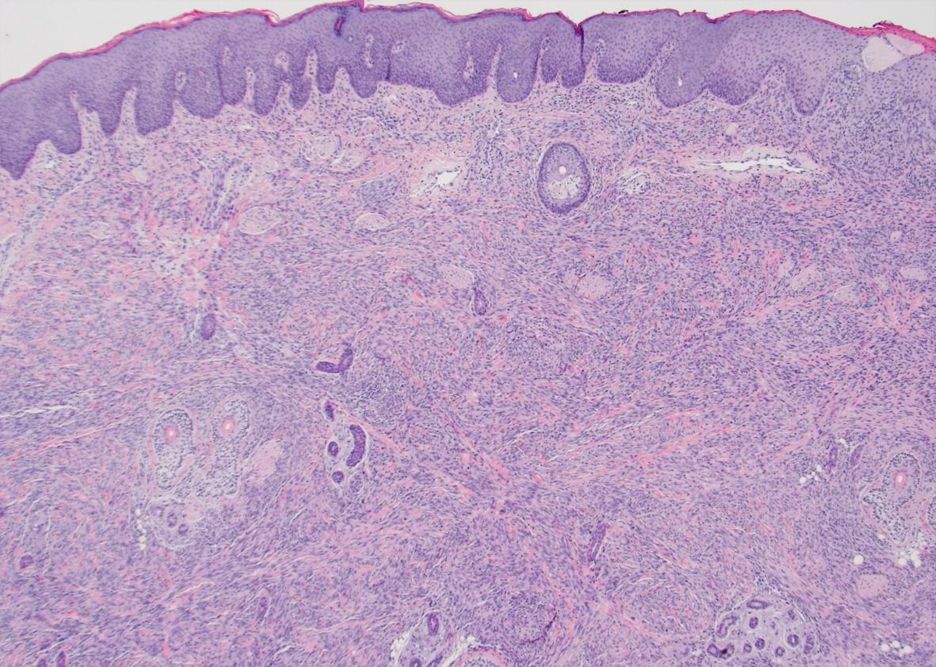
Figure 4. H&E 10x. Invasion through the deep dermis and subcutaneous layers by oval to spindled neoplastic cells arranged in intersecting fascicles and herringbone pattern. Mitosis were common.

Figure 5. H&E 10x. The cells focally invaded the fascial plane before terminating near the inked margin of resection.
References:
- Lapeña LM, Caldas MCS, Rammírez C, et al. Larotrectinib as an Effective Therapy in Congenital Infantile Fibrosarcoma: Report of Two Cases. European J Pediatr Surg Rep 2022;10:e76-e79
- Parida L, Fernandez-Pineda I, Uffman JK, et al. Clinical management of infantile fibrosarcoma: a retrospective single-institution review. Pediatr Surg Int. 2013 Jul; 29(7): 703-708.
- Han Y, Lian K, Zhang D. Treatment of infantile fibrosarcoma: A tertiary care center 60 experience. Front Pediatr. 2022; 10: 1015185. 61
About the authors
Anna Marie Johnson is a senior student at Hendrix College in Conway, AR.
Jennifer White Johnson, MD is a pediatrician at Johnson Dermatology in Fort Smith, AR.
Brad Russell Johnson MD, is a dermatologist and dermatologic surgeon at Johnson Dermatology in Fort Smith, AR.
Laura Gonzalez-Krellwitz, MD, is an Assistant Professor of Pediatric Pathology at Arkansas Children’s Hospital in Little Rock, AR.
Patricia Connor, MD is a pathology resident at the University of Arkansas for Medical Sciences in Little Rock, AR.
Sandra Marchese Johnson MD, FAAD is a dermatologist at Johnson Dermatology in Fort Smith, AR.
Consent for the publication of all patient photographs and medical information was provided by the authors at the time of article submission to the journal stating that all patients gave consent for their photographs and medical information to be published in print and online and with the 18 understanding that this information may be publicly available.