With Maritza I. Perez, MD

“Hispanics are a pool of people that have all skin types, from Fitzpatrick I through VI.” And when it comes to skin cancer risk, people—including Hispanics themselves—seem to bundle everyone who speaks Spanish or comes from a Spanish-speaking country into one homogenous group.
The heterogeneity of skin types in Hispanic Americans makes it challenging to draw conclusions about skin cancers in this population. When these patients do develop skin cancers, they generally fare worse than Caucasians with similar cancers. Tackling such inequities requires battling misconceptions among Hispanic Americans and dermatologists themselves.1
A dearth of research makes it difficult to establish incidence rates for skin cancers in Hispanic Americans, said Dr. Perez, a professor of dermatology and Mohs surgery director at UConn Health/the University of Connecticut Medical Center in Farmington, Conn.
For non-melanoma (keratinocytic) skin cancers, a single-center study showed a rate of 3%, with cancers mainly affecting younger females compared to Caucasian and Asian patients.2 Incidence rates of keratinocytic skin cancers in the latter groups are 20% to 30% and 2% to 4%, respectively, she said.
“The melanoma situation is a little more complicated because it depends on if you’re looking at the whole United States or just 2 locations.” Nationally, melanoma incidence per 100,000 among Hispanics (4.8) falls between rates of Caucasians (27.2) and Asians/African-Americans (1.0 to 1.4).3 In the past 2 decades, said Dr. Perez, melanoma incidence among Hispanics has risen by 20%.4
National figures may be misleading, she said, because two-thirds of the US Hispanic population lives in California, Texas, Florida, New York, and Illinois. A Florida study showed that between 1992 and 2004, Hispanic men faced a 20% higher risk of invasive melanoma than male peers elsewhere.5 A registry study performed in Florida showed that between 1990 and 2004, Hispanic patients faced a higher risk of regional or distant metastases at diagnosis (18%) than non-Hispanic whites (12%).6
Similar dynamics exist in California, said Dr. Perez. Epidemiological research conducted there reflects a higher melanoma burden among Hispanics versus non-Hispanic whites.7 The foregoing study moreover showed an especially high burden and worse prognosis in Hispanics of lower socioeconomic status (SES), particularly men, versus their Caucasian peers. Additional studies link low SES in Hispanic patients in California and nationally with thicker tumors at diagnosis and worse outcomes.8,9,10
“So at least in 2 states,” said Dr. Perez, “we can document that the incidence of melanoma is higher in Hispanics.” She attributes the poor prognosis of melanoma in Hispanic patients partly to the melanomas’ nodular nature. “That’s why survival is lower and advanced disease is more common—they happen to get the worst melanomas.”
Horizontal growth such as that of lentigo maligna or superficial spreading melanoma is considered curable, explained Dr. Perez. “But once there is vertical growth and the melanoma invades the dermis, the prognosis decreases significantly.”
Researchers have attributed poorer skin cancer outcomes among Hispanic patients to factors ranging from lower health insurance access to a lack of culturally targeted screening.11 “In reality,” said Dr. Perez, “everything is related to acculturation and the way that Hispanics perceive themselves. Hispanics have decided that for some reason, they are not at risk of skin cancer.”12,13,14
Hispanic-American patients more likely will believe that they can develop skin cancer when the message comes from Hispanic doctors, said Dr. Perez. “That’s why we need more Hispanic dermatologists. We know that patients relate more to doctors that look, think, and feel like them.”
Unfortunately, she added, many dermatologists appear to share Hispanic patients’ misconceptions. Diagnosing nodular melanoma in any patient requires a keen eye, she said. “If you don’t have that index of suspicion because your patient is Hispanic, then you’re not going to think about it.”
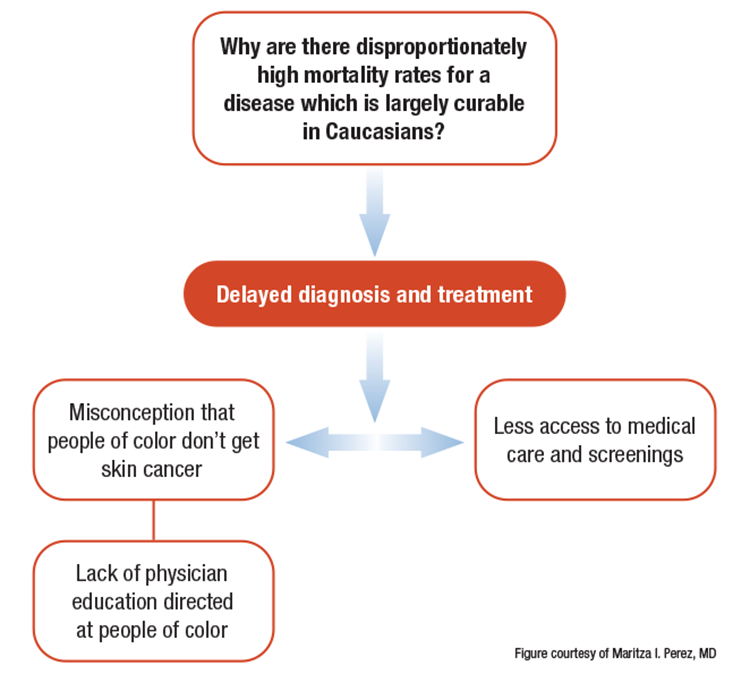
No study documents dermatologists’ lack of awareness regarding skin cancer in Hispanic patients, said Dr. Perez. Rather, it is her observation—based on 41 years’ experience working in New England, Puerto Rico, and Florida—that many dermatologists do not believe such patients are at risk for skin cancers including melanoma.
The challenge for Dermatologists, then, is less about weighing specific treatment modalities in skin of color (SOC) than raising awareness, she said. “There’s not a campaign for total skin evaluation for Hispanics because the preconception is that they will not get skin cancer.” Accordingly, groups including the Skin of Color Society and the American Academy of Dermatology (AAD) Task Force on Skin Cancer and Skin of Color (both of which Dr. Perez is a member), educate dermatologists and the public about the potential for skin cancer in darker-skinned patients including Hispanic patients.
Still, she has found it difficult to advance SOC-related topics in academic publishing. For starters, she said, dividing the world’s entire population into 6 Fitzpatrick skin types oversimplifies the reality. “But until we have a better skin-color palette, that’s what we have as a reference.” Dr. Perez has been working on such a project, which she said will take at least another year to complete and publish. Additionally, the AAD task force has been working for 2 years on an article about sun protection recommendations for SOC. “It’s going to take at least another year. This is a very difficult task.”
In the past, she said, publishing research regarding SOC has not been a priority for journals that cover dermatology as a whole. “It’s not a complaint—it’s reality. Many of us who work in the field of skin of color and try to publish in the journals find it’s not welcome because it’s not for the general population.”
On a broader scale, Dr. Perez recommended that all dermatologists start teaching children of all races in middle and high school about their potential for skin cancer and the need for sun protection. “It’s education—so that when they grow up, they will understand that they are prone to it, and they can protect themselves. Both the Hispanic population and the dermatologists in the United States have to understand that Hispanics really are at risk of skin cancer, specifically melanoma, in the Sunbelt areas.”
Erasing the misconception that Hispanic patients are immune will raise dermatologists’ clinical suspicion level and convince Hispanic American patients to take measures such as avoiding sun exposure, seeing doctors regularly, and performing skin self-examinations, she said.
REFERENCES:
1. Perez MI. Skin cancer in Hispanics in the USA. Mark Allen Everett, MD, Skin of Color Symposium; April 23, 2021; Oklahoma City, OK.
2. Loh TY, Ortiz A, Goldenberg A, Brian Jiang SI. Prevalence and clinical characteristics of nonmelanoma skin cancers among Hispanic and Asian patients compared with white patients in the United States: a 5-year, single-institution retrospective review. Dermatol Surg. 2016;42(5):639-645.
3. Howlader N, Noone AM, Krapcho M, et al. (eds). SEER Cancer Statistics Review, 1975-2017. https://seer.cancer.gov/archive/csr/1975_2017/results_merged/sect_16_melanoma_skin.pdf. Published April 2020. Accessed June 8, 2021.
4. Perez MI. Hispanic doesn’t mean immune to skin cancer. Skin Cancer Foundation. Https://www.skincancer.org/blog/hispanic-doesnt-mean-immune-to-skin-cancer/. Published October 14, 2020. Accessed June 9, 2021.
5. Rouhani P, Pinheiro PS, Sherman R, et al. Increasing rates of melanoma among nonwhites in Florida compared with the United States. Arch Dermatol. 2010;146(7):741-746.
6. Hu S, Parmet Y, Allen G, et al. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145(12):1369-1374.
7. Pollitt RA, Clarke CA, Swetter SM, Peng DH, Zadnick J, Cockburn M. The expanding melanoma burden in California Hispanics: importance of socioeconomic distribution, histologic subtype, and anatomic location. Cancer. 2011;117(1):152-161.
8. Cockburn MG, Zadnick J, Deapen D. Developing epidemic of melanoma in the Hispanic population of California. Cancer. 2006;106(5):1162-1168.
9. Garnett E, Townsend J, Steele B, Watson M. Characteristics, rates, and trends of melanoma incidence among Hispanics in the USA. Cancer Causes Control. 2016;27(5):647-659.
10. Harvey VM, Oldfield CW, Chen JT, Eschbach K. Melanoma disparities among US Hispanics: use of the social ecological model to contextualize reasons for inequitable outcomes and frame a research agenda. J Skin Cancer. 2016; 2016:4635740. doi:10.1155/2016/4635740
11. Perez MI. Skin cancer in Hispanics in the United States. J Drugs Dermatol. 2019;18(3):s117-s120.
12. Kim M, Boone SL, West DP, Rademaker AW, Liu D, Kundu RV. Perception of skin cancer risk by those with ethnic skin. Arch Dermatol. 2009;145(2):207-208.
13. Ma F, Collado-Mesa F, Hu S, Kirsner RS. Skin cancer awareness and sun protection behaviors in white Hispanic and white non-Hispanic high school students in Miami, Florida. Arch Dermatol. 2007;143(8):983-988.
14. Torres SM, Ramos M, Leverence R, Bowen D, Berwick M, Hay J. A pilot study of skin cancer risk reduction behaviors, cancer communication, and skin cancer beliefs in Hispanics. Calif J Health Promot. 2014;12(1):95–100.
DISCLOSURES:
Dr. Perez is a consultant for Procter & Gamble, L’Oreal, and Galderma.
Physician contact info: mperez@adv-aesthetics.com, 203-972-7546, 203-984-3101 cell


