Residual inflammation in psoriasis patients may lead to obesity and fatty liver disease, and this inflammation may linger even when skin responds well to treatment with biologics.
The findings, which appear in the Journal of Investigative Dermatology (JID), suggest that addressing the systemic inflammatory burden beyond skin symptoms in psoriasis, potentially with interventions targeting obesity and metabolic dysfunction, may improve overall patient outcomes.
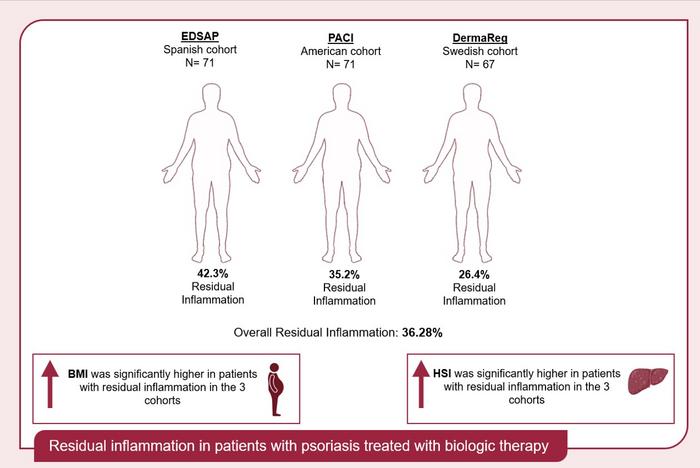
This prospective observational study assessed residual inflammation in 209 psoriasis patients across three international cohorts (Spain, USA, and Sweden) who had achieved a ≤ 2 on the Psoriasis Area Severity Index (PASI), indicating no or mild psoriasis on stable biologic therapy.
Residual inflammation was present in 36.3% of these patients and was significantly linked to higher BMI, metabolic dysfunction-associated steatotic liver disease (MASLD), increased baseline systemic inflammation, and greater adipose tissue, the study showed.
Insights into Psoriasis Management
“Our present study offers novel insights into psoriasis management by characterizing residual inflammation in patients undergoing biologic therapy across three independent international cohorts,” says lead investigator Álvaro González-Cantero, MD, PhD, of the Department of Dermatology at the Hospital Universitario Ramón y Cajal and a member of the Faculty of Medicine at the Universidad Francisco de Vitoria in Madrid, in a news release.
“This is particularly important now because it highlights that despite achieving good skin responses with biologics, a significant subset of patients, predominantly those with obesity (especially central obesity), higher baseline systemic and organ inflammation (as shown by PET/CT), increased subcutaneous and visceral adipose tissue, and markers of MASLD, continue to exhibit residual inflammation.”
The findings underscore “a critical unmet need to address the systemic inflammatory burden beyond skin symptoms in psoriasis, potentially requiring interventions targeting obesity and metabolic dysfunction to improve overall patient outcomes,” he says.
Co-first author Alba Lecumberri, MD, of the Department of Dermatology at the Hospital Universitario Ramón y Cajal in Madrid, notes, “The strong association identified between residual inflammation and obesity, particularly central obesity and markers of hepatic inflammation, suggests that these patients may benefit from a more intensive cardiovascular risk assessment and management. This could involve closer monitoring of inflammatory markers like high-sensitivity C-reactive protein, as well as parameters related to liver health, by integrating lifestyle modifications or weight management strategies, potentially leading to earlier detection and intervention for associated comorbidities.”
Elevated Cardiovascular Risk
Commenting on the study, Michael Garshick, MD, MBBS, of the Department of Medicine at the New York University Grossman School of Medicine in New York, NY, adds, “This research emphasizes the elevated cardiovascular risk in patients with psoriasis and that dermatologists (and rheumatologists) should be at the forefront of recognizing the cardiometabolic and cardiovascular concerns in the psoriasis patient population. An elevated high-sensitivity C-reactive protein testing can be used to further refine assessment of which psoriasis may be candidates for both lipid lowering and weight loss treatments.”
The investigators point out that further studies are needed to confirm their findings and better understand the long-term implications for patient management.
Co-first author Emilio Berna-Rico, MD, PhD, Department of Dermatology, Hospital Universitario Ramón y Cajal, Madrid, concludes, “We believe this to be a relevant study for dermatology, as it has assigned the term ‘residual inflammation’ for the first time in psoriasis patients, taking into account the systemic inflammation of the disease. We hope that our results can pave the way for a broader approach in psoriasis research, which will allow us to mitigate the effects of systemic inflammation and improve patient management through the use of the innovative therapies available to us, in addition to educating patients on a healthy and anti-inflammatory lifestyle, in collaboration with other healthcare professionals.”
Joel M. Gelfand, MD, MSCE, of the Department of Dermatology at the University of Pennsylvania Perelman School of Medicine, and JID Deputy Editor for Clinical Research & Epidemiology, adds, “Despite excellent control of skin disease, a substantial percentage of psoriasis patients demonstrate residual systemic inflammation. These findings emphasize that just treating the skin signs of psoriatic disease is not sufficient, and patients often need additional approaches to lowering systemic inflammation.”