PEDIATRIC DERMATOLOGY
The clinical speculation that use of hair oil may increase the rate of TINEA CAPITIS IN AFRICAN-AMERICAN CHILDREN does not seem to be valid. Moreover, use of cosmetic hair oil has minimal impact on the sensitivity of a fungal culture for tinea capitis.

Therefore, diagnosis and treatment of tinea capitis may proceed along standard lines, regardless of whether or not hair oil is routinely applied to the scalp. To read more: Wichterman C, Kumar MG. Bayliss SJ. Influence of hair oil on scalp fungal cultures. Pediatr Dermatol. 2020;37(5):977-978. https://pubmed.ncbi.nlm.nih.gov/32757310/
INFECTIOUS DISEASES
Compression therapy may help reduce the likelihood of new CELLULITIS episodes in patients with leg edema and multiple prior episodes of lower extremity cellulitis.

To read more: Webb E. Compression therapy to prevent recurrent cellulitis of the leg. N Engl J Med. 2020;383(7):630-63. https://pubmed.ncbi.nlm.nih.gov/32786188/
HIV-positive individuals who reliably take ANTI-RETROVIRAL THERAPY (ART) and achieve viral suppression (defined as HIV-1 RNA <200 copies per mL) do not transmit the virus to uninfected contacts, despite condomless sex. This supports the supposition that “undetectable equals untransmittable” and underscores the importance of adherence to ART regimens. To read more: Rodger AJ, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393:2428-2438. https://pubmed.ncbi.nlm.nih.gov/31056293/
Adapalene gel 0.1% applied twice daily for 4 weeks may adequately treat TINEA VERSICOLOR. Moreover, this therapy is equipotent to ketoconazole cream 2% applied in a similar regimen. To read more: Bakr E, et al. Adapalene gel 0.1% vs ketoconazole cream 2% and their combination in treatment of pityriasis versicolor: A randomized clinical study. Dermatol Ther. 2020;33(3):e13319.
Based on a large-scale Danish cohort study over 10 years, exposure to ORAL TERBINAFINE during pregnancy does not lead to an increased risk of either congenital malformations or spontaneous abortion. To read more: Andersson NW, et al. Evaluation of association between oral and topical terbinafine use in pregnancy and risk of major malformations and spontaneous abortion. JAMA Dermatol. 2020;156(4):375-383. https://pubmed.ncbi.nlm.nih.gov/32129793/
RHEUMATOLOGIC DISEASES
Mycophenolate mofetil, at standard doses, may be beneficial for the management of MORPHEA. This is true even in cases of refractory generalized or linear morphea. To read more: Arthur M, et al. Evaluation of the effectiveness and tolerability of mycophenolate mofetil and mycophenolic acid for the treatment of morphea. JAMA Dermatol. 2020;156(5):1-8. https://pubmed.ncbi.nlm.nih.gov/32236497/
ADULT-ONSET DERMATOMYOSITIS carries some risk of associated internal neoplasia. When anti-transcriptional intermediary factor-1γ (anti-TIF-1γ) antibody is present, there is a 9 times greater risk of cancer than when this autoantibody is absent.

However, some 60% of those who are positive will remain cancer-free. Dermatomyositis patients who are anti-TIF-1γ positive should undergo a thorough evaluation for cancer, even though many will not have occult neoplasia. To read more: Best M. Use of anti-transcriptional intermediary factor-1 gamma autoantibody in identifying adult dermatomyositis patients with cancer: a systematic review and meta-analysis. Acta Derm Venereol. 2019;99(3):256-262. https://pubmed.ncbi.nlm.nih.gov/30460368/
TNF-inhibitors and low-dose IL-17 inhibitors respond normally to killed virus influenza vaccine injection. If possible, those taking METHOTREXATE should stop the drug for 2 weeks after influenza vaccine administration to maximize seroprotective titers. About half of those on cyclosporine will not achieve protective titers. There are not enough data to comment on interaction between IL-23 inhibitors and influenza vaccination. To read more: Kim JY, Dao H. Influenza vaccination recommendations during use of select immunosuppressants for psoriasis. Cutis. 2020;106:194-195. https://pubmed.ncbi.nlm.nih.gov/33186429/
PSORIASIS
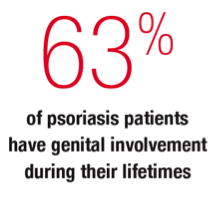
GENITAL PSORIASIS may be less scaly than disease elsewhere, but may be accompanied by pain, itching, or burning. To read more: Cather JC, et al. Patients’ perspectives on the impact of genital psoriasis: a qualitative study. Dermatol Ther (Heidelb). 2017;7:447-461.
https://pubmed.ncbi.nlm.nih.gov/29076000/
The only biologic drug specifically approved for GENITAL PSORIASIS is IXEKIZUMAB, although the entire gamut of topical and system drugs may be employed based upon patient preferences and prior experiences. To read more: Ryan C, et al. Efficacy and safety of ixekizumab in a randomized, double-blinded, placebo-controlled phase IIIb study of patients with moderate-to-severe genital psoriasis. Br J Dermatol. 2018;179:844-852. https://pubmed.ncbi.nlm.nih.gov/29747232/
A prospective German study strongly suggests that PSORIASIS, regardless of body surface area affected, is associated with an increased risk of severe PERIODONTITIS. Patients with psoriasis should be encouraged to get regular dental examinations. To read more: Woeste S, et al. Oral health in patients with psoriasis—a prospective study. J Invest Dermatol. 2019;139(6):1237-1244. https://pubmed.ncbi.nlm.nih.gov/30610840/
FACIAL PSORIASIS is associated with severe overall disease and early age of onset. Interestingly, the pinna is quite often involved compared to other facial sites. To read more: Passos AN, et al. Facial involvement and the severity of psoriasis. Int J Dermatol. 2019;58(11):1300-1304. https://pubmed.ncbi.nlm.nih.gov/31347152/
COSMETIC DERMATOLOGY
Does ingestion of ORAL COLLAGEN do anything? A meta-analysis of 11 randomized controlled studies suggests that it does. Both collagen hydrolysate (2.5-10.0g/day x 8-24 weeks) and collagen tripeptide (3g/day x 12 weeks) were beneficial. Both, for example, decreased xerosis and increased elasticity. Larger, longitudinal studies are needed. However, it does appear that oral collagen ingestion may carry some cutaneous benefits. To read more: Choi FD, et al. Oral collagen supplementation: a systematic review of dermatological applications. J Drugs Dermatol. 2019;18(1):9-16. https://pubmed.ncbi.nlm.nih.gov/30681787/
COVID-19
The COVID-19 PANDEMIC has severely disrupted the medical care system’s ability to screen for and detect cancer in the United States. Among the largest decreases in medical encounters related to the diagnosis of neoplasia during the pandemic include malignant melanoma, prostate cancer, and breast cancer. To read more: London JW, et al. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;4:657-665. https://pubmed.ncbi.nlm.nih.gov/32716647/
DRUGS AND DEVICES
SYSTEMIC 5-FLUOROURACIL (5-FU) is indicated for the treatment of adenocarcinoma of colon/rectum, stomach, pancreas, and breast. Systemic 5-FU can cause intense, but reversible, palmar hyperpigmentation. To read more: Schaefer JK and Ramnath N. Fluorouracil-induced hyperpigmentation. N Engl J Med. 2020;382(4):e6. https://pubmed.ncbi.nlm.nih.gov/31971682/
ROSACEA
A German case-control study demonstrated that the risk of developing RHINOPHYMA correlates with higher alcohol intake. This association is especially true if the patient is also diabetic or has a family history of rhinophyma.

To read more: Second J, et al. Rhinophyma is associated with alcohol intake. J Am Acad Dermatol. 2019;81(1):249-250. https://pubmed.ncbi.nlm.nih.gov/30630023/
CONTACT DERMATITIS
A large-scale Korean study suggests that hidradenitis suppurativa is associated with about a 28% excess risk of cancer, perhaps due to chronic inflammation and an aberrant immune response. Specifically, Hodgkin lymphoma, oral cavity cancer and pharyngeal cancer, central nervous system cancer, and prostate cancer had at least twice the incidence among those with hidradenitis when compared to a matched case-control population. To read more: Jung JM, et al. Assessment of overall and specific cancer risks in patients with hidradenitis suppurativa. JAMA Dermatol. 2020;156(8):1-10. https://pubmed.ncbi.nlm.nih.gov/32459291/
En bloc SURGICAL REMOVAL OF HIDRADENITIS SUPPURATIVA-AFFECTED AREAS is a viable option in the management of this disorder. Despite a high recurrence rate of about 35%, most patients prefer surgical management over medical management, given the current methods available to accomplish the latter. To read more: Fertitta L, et al. Efficacy and satisfaction of surgical treatment for hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2020;34(4):839-845. https://pubmed.ncbi.nlm.nih.gov/31799758/
SECONDARY SQUAMOUS CELL CARCINOMA may occur in the setting of HIDRADENITIS SUPPURATIVA. Despite seemingly adequate wide local excision, cancer recurrence is common, often leading to death. To read more: Kohorst JJ, et al. Squamous cell carcinoma in perineal, perianal, and gluteal hidradenitis suppurativa: experience in 12 patients. Dermatol Surg. 2019;45(4):519-526. https://pubmed.ncbi.nlm.nih.gov/30608295/
GENERAL DERMATOLOGY
A recent analysis of just over 2000 American adults demonstrated a TATTOO prevalence of 32%. About 50% of the tattoos were in normally visible sites. In this particular study, there was a statistically significant association between tattoo placement and mental health issues, sleep abnormalities, smoking, jail time, and increased number of sex partners. The presence of tattoos may alert the clinician to the possibility of problematic behavior. To read more: Mortensen K, et al. Are tattoos associated with negative health-related outcomes and risky behaviors? Int J Dermatol. 2019;58(7):816-824. https://pubmed.ncbi.nlm.nih.gov/30677140/
When prescribing TOPICAL CORTICOSTEROIDS, don’t assume the dispensing pharmacy will provide precisely the product you request, in the quantity you desire and with the instructions you prefer. Be aware that the amount of medication dispensed is often less than that prescribed, and patients may be told to discontinue treatment long before intended. Warn the patient that, should those things occur, to contact you so that you may discuss the situation with the pharmacist. To read more: Millard AN, Stratman EJ. Assessment of topical corticosteroid prescribing, counseling, and communication among dermatologists and pharmacists. JAMA Dermatol. 2019;155(7):838-843. https://pubmed.ncbi.nlm.nih.gov/30916731/
A large-scale retrospective European study demonstrated that chronic use of TOPICAL CORTICOSTEROIDS is associated with an increased risk of developing Type 2 diabetes (T2D). There was a dose-response relationship between new onset T2D and the potency of topical steroids being used. Be careful with topical steroid use in those with a family history of diabetes or existent borderline hyperglycemia. To read more: Andersen YMF, et al. Association between topical corticosteroid use and type 2 diabetes in two European population-based adult cohorts. Diabetes Care. 2019;42(6):1095-1103. https://pubmed.ncbi.nlm.nih.gov/30936111/
Only 12% of the American allopathic MEDICAL SCHOOLS have a dermatology-specific course in the preclinical curriculum and only 1% have a required dermatology rotation in the third or fourth year of training. Dermatologic skills are not widely taught in medical schools. To read more: Cahn BA, et al. Current status of dermatologic education in US medical schools. JAMA Dermatol. 2020;156(4):468-470. https://pubmed.ncbi.nlm.nih.gov/32101260/
Patients receiving EPIDERMAL GROWTH FACTOR RECEPTOR INHIBITORS for the treatment of cancer are prone to develop severe acneiform eruptions. This adverse event may be prevented or lessened in severity by prophylactic administration of oral tetracycline derivatives at typical therapeutic doses. To read more: Yu Z, et al. Evaluation of a comprehensive skin toxicity program for patients treated with epidermal growth factor receptor inhibitors at a cancer treatment center. JAMA Dermatol. 2020;e201795. https://pubmed.ncbi.nlm.nih.gov/32609305/
Studies show that VISIBLE SKIN ABNORMALITIES may evoke strong negative reactions from others. This may lead to everything from stares to verbal insults to online harassment. Males and those who have no association with healthcare are most likely to react negatively to abnormal skin. You may have to help your patients cope with this social ostracism. To read more: Pereira PA, et al. Aversion caused by skin diseases: a crowdsourcing study. Int J Dermatol. 2019;58(1):60-66. https://pubmed.ncbi.nlm.nih.gov/30229877/
Patients may have easy access to low-cost, ultrapotent TOPICAL CORTICOSTEROIDS manufactured overseas by purchasing them at local stores and shops specializing in “foreign products.” To read more: Kimyon RS, et al. Prescription-strength topical corticosteroids available over the counter: Cross-sectional study of 80 stores in 13 United States cities. J Am Acad Dermatol. 2020;82(2):524-525. https://pubmed.ncbi.nlm.nih.gov/31672686/
CUTANEOUS ONCOLOGY
Patients who experience significant DISCOMFORT DURING THE INJECTION OF LOCAL ANESTHETIC may be made more comfortable via use of localized vibration delivered to the surrounding area. This strategy to mitigate pain during injection works best in the head and neck region and among individuals over the age of 65. To read more: Govas P, et al. Effect of a vibratory anesthetic device on pain anticipation and subsequent pain perception among patients undergoing cutaneous cancer removal surgery: A randomized clinical trial. JAMA Facial Plast Surg. 2019;21(6):480-486. https://pubmed.ncbi.nlm.nih.gov/31513234/
SURGICAL GLUES, based on n-butyl or 2-octyl cyanoacrylate, are durable, flexible, watertight, bactericidal, and afford excellent cosmesis. However, there is a risk of allergic contact dermatitis associated with surgical glue application. To read more: Nigro LC, et al. Should we stick with surgical glues? The incidence of dermatitis after 2-octyl cyanoacrylate exposure in 102 consecutive breast cases. Plast Reconstr Surg. 2020;145(1):32-37. https://pubmed.ncbi.nlm.nih.gov/31881600/
Intralesional injection of classic KERATOACANTHOMAS WITH METHOTREXATE leads to almost as frequent a complete remission as surgical excision. Consider intralesional methotrexate in: areas which might be difficult to close following removal, areas which may not heal readily or well, or when there is a plethora of such lesions. To read more: Moss M, et al. Management of keratoacanthoma: 157 tumors treated with surgery or intralesional methotrexate. Dermatol Surg. 2019;45(7):877-883. https://pubmed.ncbi.nlm.nih.gov/30608293/
ATOPIC DERMATITIS
A meta-analysis of 15 studies including more than 310,000 patients demonstrated that patients with ATOPIC DERMATITIS ARE AT RISK FOR SUICIDAL IDEATION and suicide attempts. To read more: Sandhu JK, et al. Association between atopic dermatitis and suicidality: a systematic review and meta-analysis. JAMA Dermatol. 2019;155(2):178-18. https://pubmed.ncbi.nlm.nih.gov/30540348/
Pain is a distinct symptom associated with atopic dermatitis. 61% of US adults with active atopic dermatitis report pain; 33% at least weekly and 5% daily. The occurrence of pain correlates, overall, with the severity of atopic dermatitis. To read more: Silverberg JI, et L. Pain is a common and burdensome symptom of atopic dermatitis in United States adults. J Allergy Clin Immunol Pract. 2019;7(8):2699-2706. https://pubmed.ncbi.nlm.nih.gov/31228619/
Based upon a large US cohort study, there does not appear to be an increased risk of non-melanoma skin cancer among adults with ATOPIC DERMATITIS who utilize topical calcineurin inhibitors. This holds true regardless of which drug is employed and is not related to frequency and duration of use. To read more: Asgari MM, et al. Association between topical calcineurin inhibitor use and keratinocyte carcinoma risk among adults with atopic dermatitis. JAMA Dermatol. 2020;Aug 12. https://pubmed.ncbi.nlm.nih.gov/32785626/
Despite a black-box warning, a large-scale observational study of more than 7 years duration failed to demonstrate an increased risk of non-melanoma skin cancer among adult ATOPIC DERMATITIS patients exposed to topical calcineurin inhibitors (TCI). Control comparison group included those exposed to topical cortico-steroids (TCS) or neither TCI nor TCS. To read more: Asgari MM, et al. Association between topical calcineurin inhibitor use and keratinocyte carcinoma risk among adults with atopic dermatitis. JAMA Dermatol. 2020;Aug 12. https://pubmed.ncbi.nlm.nih.gov/32785626/
Based upon-large scale European studies, there may not be an increased risk of cancer among ATOPIC DERMATITIS patients. To read more: Mansfield KE, et al. Association between atopic eczema and cancer in England and Denmark. JAMA Dermatol. 2020;Aug 12. https://pubmed.ncbi.nlm.nih.gov/32579178/


