Pearls for optimally managing hyperhidrosis
By Lisette Hilton; Reviewed by Dee Anna Glaser, MD
With a growing list of hyperhidrosis treatment options, it is becoming more important that dermatologists understand how to optimally use individual therapies, combine treatments, and minimize side effects to improve patients’ quality of life, according to Dee Anna Glaser, MD, president and founding member of the International Hyperhidrosis Society and professor and interim chair of Dermatology at St. Louis University School of Medicine.

Hear the full interview at www.thedermdigest.com/glaser_podcast
Dr. Glaser, who presented on hyperhidrosis at the Fall Clinical Dermatology Conference in 2020, shared treatment pearls from that talk with The Dermatology Digest.
Look beyond sweat to recommend individualized treatment
Dermatologists have limited options for treating and managing hyperhidrosis. “You can use topical antiperspirants. There is the new topical glycopyrronium cloth. There are old favorites like iontophoresis devices, botulinum toxin, and oral medications, which can be used off label. There are local [surgical] procedures, and microwave thermolysis is an FDA-cleared device,” Dr. Glaser said.
Sometimes, a therapy that seems ideal initially is not. Dr. Glaser described a young man with severe hyperhidrosis involving his face, scalp, and underarms. He had excessive sweating of the back, chest, groin, palms, and soles.
A patient with multiple excessive sweating sites would appear to be an ideal candidate for systemic therapy. But this patient worked outdoors and played sports and needed to sweat to regulate body temperature, she said.
Dr. Glaser and the patient decided instead to combine compounded topical anticholinergics that the patient would use on face and scalp. Those were the areas that bothered him most, which brings up another pearl: First ask each patient what bothers the patient most, so you can focus treatment on those areas, she said.
“Then, we talked about possibly adding propranolol, which can be very effective for sweating that the patient notices with a specific event—things like going on a job interview or meeting new people,” she said. “Sometimes using propranolol 30 to 60 minutes prior to that situation can really help to reduce the sweating at that time.”
Other examples of combination therapies that address specific areas of concern: microwave thermolysis for the underarms, which uses microwave technology to permanently destroy the sweat glands; and iontophoresis for excessive sweating of the hands and feet. Or using focal treatments such as botulinum toxin for underarms, forehead, and scalp, and a clinical strength antiperspirant or the glycopyrronium cloth for the underarms.
Treatment efficacy can vary with treatment location. For example, botulinum toxin injections into the axilla provide “amazingly good control,” according to Dr. Glaser.
“But when we inject it off label in the palms or forehead or scalp, it may provide good control but not that amazing type of control of the sweating,” she said.
Mitigate side effects
In some cases, the best option is an oral anticholinergic. Oral anticholinergic medications have potential side effects including dry mouth, dry eyes, enlarged pupils, constipation, bronchodilation, and more. In severe cases, oral anticholinergics can cause genitourinary symptoms.
“If it is an excessive dose of anticholinergics, patients may not even be able to urinate at all, which is an urgent situation. There are also cardiac arrythmias. For especially young or older patients, there can be side effects like confusion or excitement,” Dr. Glaser said.
When appropriate, Dr. Glaser uses glycopyrrolate because it is less likely to cross the blood-brain barrier and can mitigate side effects. Still, she educates patients that systemic therapies are likely to cause side effects that they might be able to manage with simple things. For example, drinking more water can help with dry mouth. Nasal sprays or eye drops can help with dry nasal passages or eyes. And extra fiber can help with mild constipation.
Set reasonable expectations
Improvement is the goal when managing hyperhidrosis. The way Dr. Glaser often puts it: She hopes patients’ episodes of excessive sweating will be less often and less severe and that they will feel like they sweat more like the “normal” population.
“I remind the patients with hyperhidrosis that we all sweat. It helps maintain our body temperature and all of us tend to sweat more than we want, especially when we are anxious and are in an environment that is uncomfortable for us,” she said.
Dr. Glaser determines if a patient has excessive sweating by how his or her sweating affects daily functions of living. The need for treatment is obvious in many cases.
“I have had some patients with severe palm sweating who have shorted out their electronic devices. They can’t function at work. I’ve had nurses who have had difficulty changing IV bags or giving injections,” Dr. Glaser said.
In other cases, the impact of excessive sweating on a person’s life is not so apparent. A teenager, for example, with excessive underarm sweating might spend a lot of time thinking about it and trying to hide it. “They may never raise their hand to answer a question in the classroom. They might not socialize or go on a date. It can affect all domains of quality of life for these patients,” she said.
A bright future
Among the drugs in the hyperhidrosis treatment pipeline is sofpironium bromide (Brickell), a topical, quickly metabolized anticholinergic in phase 3 research.
“The [topical anticholinergic] that we currently have is an individually packaged cloth and it has a little alcohol in it. [The packets] are easy and convenient, but the alcohol sometimes is a little bit irritating to the underarm,” she said. “[Sofpironium bromide] will be more of a cream-based topical that will reduce the chance of systemic anticholinergic side effects, so it be nice to have more than one product to choose from.”
What excites Dr. Glaser most is that dermatologists and other health care providers are developing a better understanding of hyperhidrosis’ potential impact and the need for individualized treatment.
“I think it is becoming more recognized and more accepted that this is not just a lifestyle problem but a medical condition that deserves treatment,” she said.
Dermatologists can learn more at SweatHelp.org, which offers treatment videos, examples for coding and billing, and more.
Disclosures
Dr. Glaser is an advisor or has received research funding from Allergan, Brickell, Dermira, Ferndale, Forest Research, Galderma, Miramar, Revance, Ulthera, and Unilever.
A new hyperhidrosis treatment looks promising

By Lisette Hilton; Reviewed by Joel L. Cohen, MD
Investigational sofpironium bromide gel (Brickell Biotech) offers sustained reductions in sweating severity without many of the side effects associated with systemic anticholinergic therapy for axillary hyperhidrosis, according to the study “Efficacy and safety of topical sofpironium bromide gel for the treatment of axillary hyperhidrosis: A phase II, randomized, controlled, double-blinded trial,” published in the Journal of the American Academy of Dermatology.
“We know that hyperhidrosis affects about 4% to 5% of the US population, which is more than 15 million Americans. About 10 million Americans suffer specifically from axillary hyperhidrosis. This has a significant negative impact on people’s social life and quality of life,” said study author Joel L. Cohen, MD, director of AboutSkin Dermatology as well as AboutSkin Research in Greenwood Village and Lone Tree, Colorado. “There is a lot of excitement about this particular drug and how it works.”
Sofpironium bromide is an analog of the anticholinergic agent glycopyrrolate. It is retro-metabolic, which means the molecules are designed to rapidly metabolize, limiting the risk of systemic side effects, such as dry mouth, pupil dilation, constipation, urinary retention, and more, Dr. Cohen told The Dermatology Digest.
If approved, sofpironium bromide will be in the mix of hyperhidrosis treatments among aluminum chloride topical antiperspirant agents, the topical glycopyrronium cloth, botulinum toxin, the microwave thermolysis device, and surgery.
“Sofpironium bromide is a topical designed to have specific efficacy in the eccrine, apoeccrine, and apocrine glands that we know become more mature as people hit adolescence and seem to be more of a problem in terms of stimulation for people who suffer from axillary hyperhidrosis,” he said.
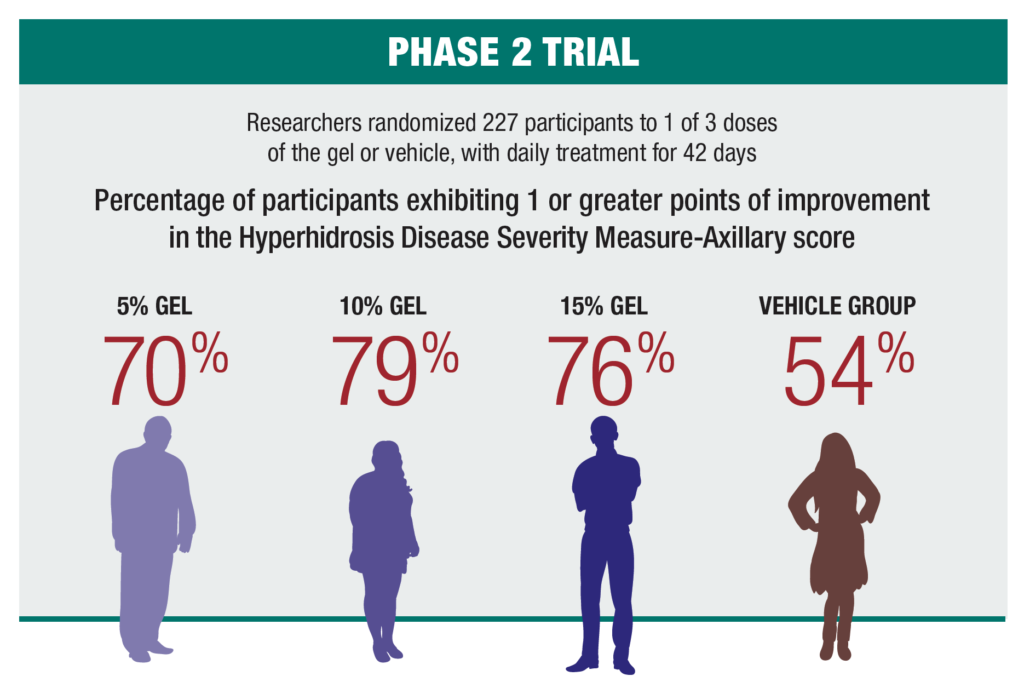
In the phase 2 trial, researchers randomized 227 participants to 1 of 3 doses of the gel or vehicle, with daily treatment for 42 days. They found the percentage of participants exhibiting 1 or greater points of improvement in the Hyperhidrosis Disease Severity Measure-Axillary score were 70% in the 5% gel group, 79% in the 10% gel group, 76% in the 15% gel group, and 54% in the vehicle group.
“In terms of the local potential skin reactions with this type of product, some people might have mild dermatitis and irritation of the skin, some may just have some redness. Some people have a little bit of itching or an eczematous type pattern,” Dr. Cohen said.
Listen for more of Dr. Cohen’s hyperhidrosis advice at www.thedermdigest.com/cohen_hyperhidrosis_podcast
US researchers began phase 3 trails looking at sofpironium bromide in October 2020.
Disclosure:
Dr. Cohen has been an investigator for Brickell Biotech.

