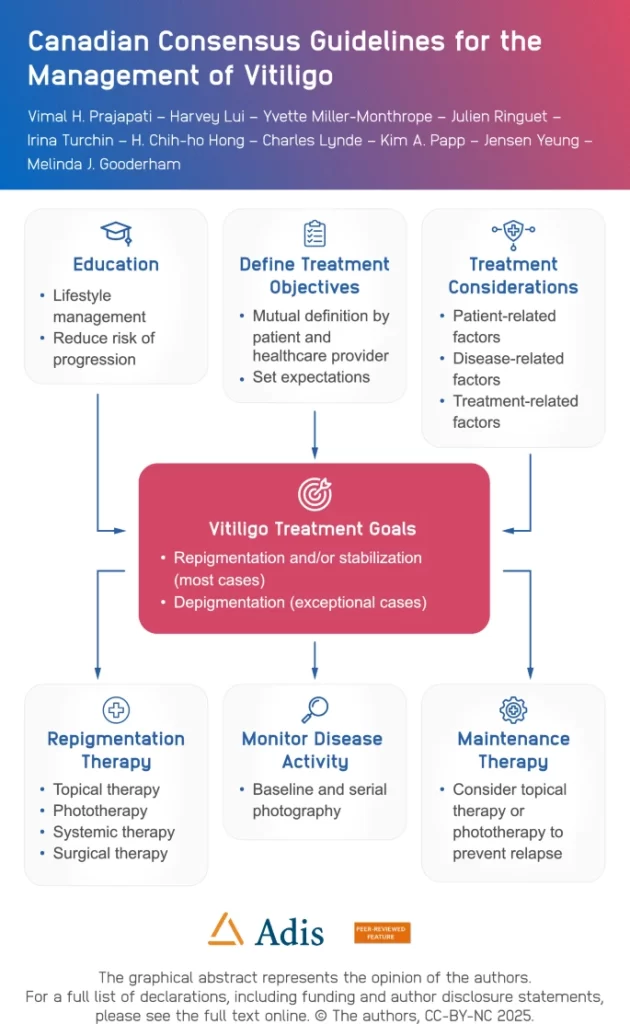
Vitiligo treatment should focus on repigmentation or stabilizing progression, rather than on depigmentation, according to new Canadian Consensus Guidelines for the Management of Vitiligo in Dermatology and Therapy.
The panel of 10 Canadian dermatologists with expertise in managing vitiligo agreed to 27 generally accepted principles, 10 consensus statements, and a treatment algorithm.
Consensus Statements
The 10 consensus statements include:
Patients with vitiligo are at a higher risk of having coexisting autoimmune disorders, including, but not limited to, thyroid disease, type 1 diabetes mellitus, alopecia areata, and pernicious anemia.
Vitiligo-specific assessment tools such as the Vitiligo Area Scoring Index (VASI), the Vitiligo Extent Score Plus (VES+), the Vitiligo Quality Of Life (VitiQOL), VIS (Vitiligo Impact Scale), and the Vitiligo Impact Patient Scale (VIPs) been used in clinical trials but are neither essential nor practical in day-to-day clinical practice.
Treatment of patients with vitiligo is directed toward repigmentation and/or stabilization.
Healthcare providers are encouraged to consider screening for concomitant autoimmune and mental health disorders in patients with vitiligo and refer to other healthcare providers when appropriate.
Maintenance therapy reduces the risk of relapse in patients with vitiligo.
Topical therapy with corticosteroids, calcineurin inhibitors, and Janus kinase (JAK) inhibitors can be considered as first-line monotherapy for the treatment of any form of vitiligo.
The off-label use of topical corticosteroids, calcineurin inhibitors, and JAK inhibitors in combination with phototherapy may be used for treating patients with vitiligo.
Phototherapy can be used alone or in combination with other therapies for the treatment of vitiligo. In exceptional cases, off-label use of systemic immunomodulatory therapies can be considered for patients with unstable or rapidly progressive vitiligo. There are currently no approved systemic therapies for vitiligo.
Although monobenzone (monobenzyl ether of hydroquinone) is approved for depigmentation therapy in the treatment of vitiligo, it should only be prescribed in exceptional circumstances by dermatologists experienced with this therapy.
“Healthcare providers will have a better understanding of patient disease burden and assessment tools for vitiligo and be better prepared to use a wide variety of treatments in conjunction with education to optimize therapeutic outcomes for their patients,” the study authors conclude.
Treatment Algorithm