Hormone-disrupting chemicals commonly found in ultra-processed food and single-use water bottles may contribute to the development of or worsen hidradenitis suppurativa (HS) in some people, according to a small study out of Johns Hopkins Medicine.
To find underlying disease pathways linking inherited and sporadic HS, the researchers compared skin samples from 12 patients with HS—who were ages 22–67 and of African American, Asian American, Hispanic American, and White heritage—to samples from eight patients without HS. They discovered that the levels of nicastrin (NCSTN), a commonly mutated gene in HS, were reduced in all participants.
Specifically, they noted NCSTN levels were low in skin fibroblasts, a known immune regulator and cell type necessary for the maintenance of connective tissues.
Based on their observations and the known association between nicastrin mutations and inflammatory skin diseases, the researchers hypothesized NCSTN loss primes fibroblasts to react intensely to pro-inflammatory biological signals, such as TNF-alpha—a known contributor to HS, psoriasis, and other inflammatory skin diseases. This results in the uncontrolled overproduction of inflammatory molecules.
“Until recently, keratinocytes were the main focus of HS research,” says Kaitlin Williams, the study’s lead author and an MD/PhD candidate in the Garza Laboratory at the Johns Hopkins University School of Medicine in Baltimore, MD. “But we were able to show that intentionally stopping NCSTN expression in non-HS fibroblasts is enough to create a reactive, pro-inflammation environment. This suggests fibroblasts may be as important as keratinocytes in the inflammatory part of this disease.”
Connecting these findings to a known association between HS and the consumption of ultra-processed foods, the researchers tested to see if the levels of plastic-associated endocrine disruptors (p-EDs) called bisphenols (eg, BPA, BPB, BPS) and phthalates (eg, DEHP, MEHP, MEP) were elevated in patients with HS and, if they were, how p-EDs possibly contributed to HS.
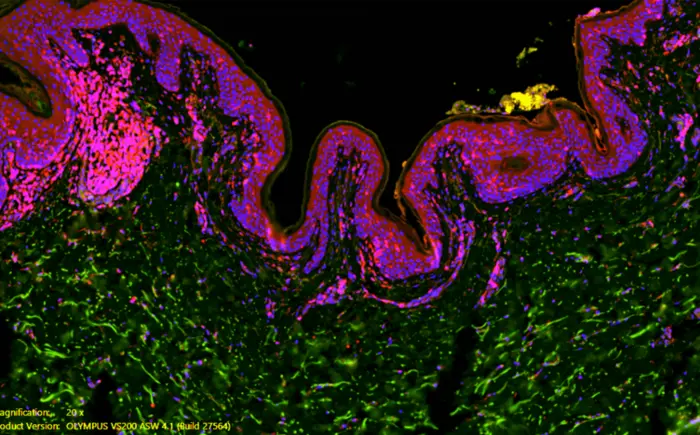
Using an imaging technique to detect the presence and location of specific chemicals in samples, researchers observed elevated levels of p-ED metabolites (molecules made by the body as it breaks down p-EDs) in the skin of HS patients vs. the non-HS control group.
The researchers then created a cocktail of eight common bisphenols and phthalates and applied them to normal fibroblasts. They discovered the p-ED cocktail lowered NCSTN levels proportionally to the concentration applied, recreating observations seen in HS samples from earlier in the study. Overall, the findings further implicate a possible role for p-EDs in some cases of HS.
The researchers hope to explore why p-EDs remain trapped in the skin at higher levels in people with HS, and whether intentionally increasing the expression of NCSTN could improve HS symptoms.
The study is published in Nature Communications.
PHOTO CAPTION: A Johns Hopkins Medicine study involving a dozen people with the inflammatory skin disease hidradenitis suppurativa (HS), which mostly affects skin folds, is believed to be the first to provide evidence that hormone-disrupting chemicals commonly found in ultra-processed food and single-use water bottles may contribute to the development of or worsen the condition in some people
PHOTO CREDIT: Kaitlin Williams, Johns Hopkins Medicine