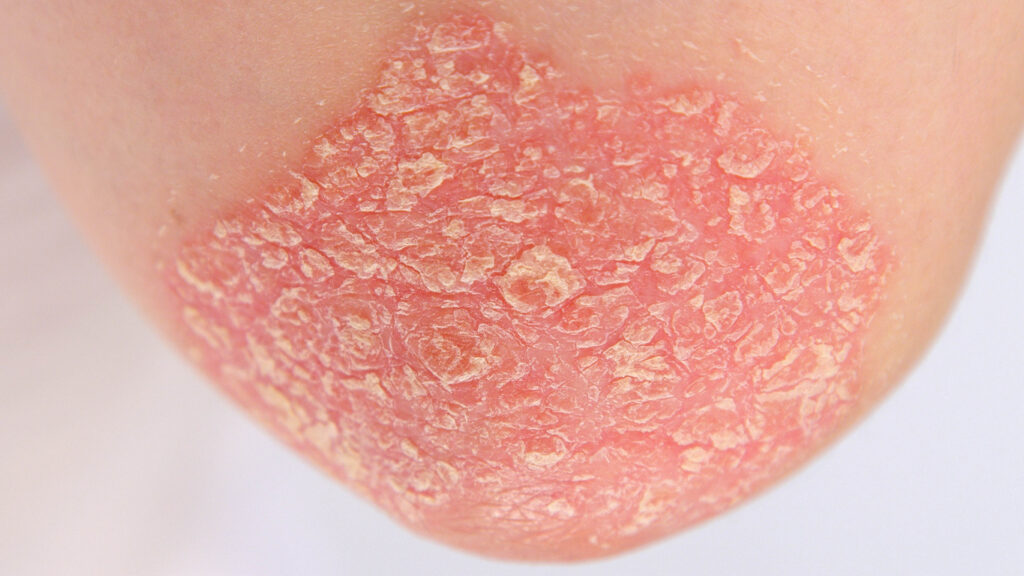
Guselkumab (Tremfya, Johnson & Johnson) is highly effective in psoriasis patients with low body surface area (BSA), moderate plaque psoriasis with involvement of special sites, according to research presented at 2025 Maui Derm Hawaii meeting.
The new study was selected as a late breaker top five finalist for the best poster Akamai Award at the meeting.
SPECTREM is an ongoing Phase 3b, multicenter, randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of guselkumab in participants with low BSA (2–15%), moderate (Investigator’s Global Assessment [IGA]=3) plaque psoriasis involving ≥1 special sites (scalp, face, intertriginous, or genital).
Overall, 338 participants were randomized 2:1 to receive guselkumab 100mg (n=225) or placebo (n=113) at Week (W)0 and W4, then every eight weeks. The primary endpoint was the proportion of participants achieving IGA0/1 (clear/minimal) at W16. Major secondary endpoints included the proportion of participants achieving Psoriasis Area and Severity Index (PASI) 90, IGA 0, and PASI 100 responses, and mean percent improvement from baseline in BSA and PASI at W16.
At baseline, mean BSA was 7.6% and mean PASI was 9.0. At W16, a significantly greater proportion of participants in the group achieved the primary endpoint (IGA0/1 response) vs. the placebo group (74.2% vs 12.4%, respectively). Results were comparable irrespective of baseline BSA, the study showed At W16, 52.9% of guselkumab -treated participants achieved PASI 90 vs. 6.2% of placebo-treated participants. Complete skin clearance (IGA 0, PASI 100) was achieved in 40.4% and 32.4% of guselkumab -treated participants vs. 3.5% and 2.7% of placebo-treated participants, respectively. At W16, mean improvements from baseline in guselkumab-treated participants were significantly greater vs. placebo-treated participants for both BSA (80.6% vs 6.1%;) and PASI (82.6% vs. 13.7%). Rates of adverse events (AEs) and serious AEs (SAEs) were generally balanced between the guselkumab and placebo groups (AEs: 37.8% vs 39.8%; SAEs: 1.3% vs 0.9%, respectively). No guselkumab-treated participants experienced AEs leading to discontinuation vs. 3.5% of placebo-treated participants. No new safety signals were identified.
“Consistent, significant improvements across multiple clearance measures irrespective of baseline BSA substantiate the effectiveness of guselkumab across a broad range of patients,” conclude the study authors who were led Linda Stein Gold, MD, Director of Clinical Research in the Department of Dermatology at Henry Ford Health in Detroit, MI.