By Krishna Patel and Peter Lio, MD
Introduction
The epithelial barrier is the first line of physical, chemical, and immunological defense against allergens, irritants, pathogens, and other environmental factors. Structural and functional integrity of the epithelial barrier is critical as damaged epithelial barriers are linked to inflammatory and autoimmune conditions.1
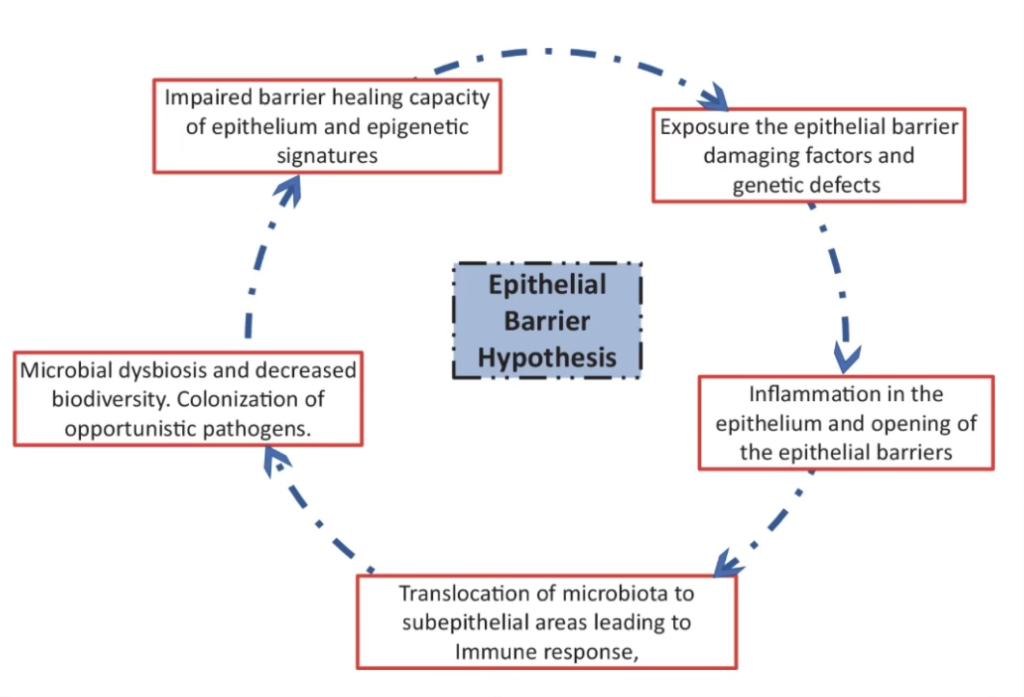
The “epithelial barrier hypothesis” proposes that genetic predisposition to epithelial barrier damage, exposure to epithelial barrier-damaging agents, and chronic epithelial inflammation are responsible for the development of allergic and autoimmune conditions. A damaged epithelial barrier can alter the microbiome through the colonization of opportunistic pathogens, local inflammation, and decreased diversity in microbiota (Figure 1). Consequently, there is a dysregulation in immune response which exacerbates inflammatory and autoimmune conditions.2 In this review, we highlight the “epithelial barrier hypothesis” proposed by Akdis, discuss the important roles of the skin, gut, and respiratory barriers, and discuss novel therapies.
Figure 1: The Epithelial Barrier Hypothesis (after Akdis CA. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat Rev Immunol. 2021;21(11):739–51.)
Skin Barrier
The epithelial barrier largely depends on the outermost layer of the epidermis, the stratum corneum. The stratum corneum consists mainly of keratinocytes and provides protection from external stimuli. Defects in the stratum corneum allow for foreign antigens, irritants, and pathogens to enter the epidermis. With stratum corneum covering most of the skin, tight junctions provide a second line of defense against the external environment. Tight junctions are composed of transmembrane proteins which are essential to the integrity of the epithelial barrier. In areas lacking stratum corneum such as hair follicles and sweat glands, tight junctions serve as the primary barrier in protecting the epithelia. Impairment in tight junction expression has been shown to contribute to the barrier dysfunction observed in patients with atopic dermatitis.3 Emollient enhancement, neonatal moisturizer, and barrier lipid replacement have all been discussed as epithelial barrier-protecting agents that may treat and possibly even prevent atopic dermatitis.4,5,6
Gut Barrier
The intestinal barrier is a selectively permeable barrier meaning it allows for the absorption of nutrients, electrolytes, and water while defending against the entry of toxins and antigens. Through desmosomes, adherens junctions, and tight junctions, the intestinal barrier maintains this selective permeability. Disrupted intestinal barrier function has become increasingly associated with the development of autoimmune and inflammatory diseases.7 Gut barrier defects have been observed in patients with systemic lupus erythematosus as well as rheumatoid arthritis. Interactions between the gut microbes and the host were found to be significant in the development of systemic lupus erythematosus.8 Gut barrier leakiness was found to be linked to rheumatoid arthritis development via increased levels of serum zonulin as well as the migration of inflammatory cells from the gut to the joints.9 Additionally, children with atopic dermatitis often have accompanying gastrointestinal symptoms due to the disruption of the intestinal barrier integrity. Probiotic supplementation such as Lactobacillus spp was shown to stabilize the intestinal barrier and improve gastrointestinal symptoms in children with atopic dermatitis.10 Recently, retinoic acid has also been shown to strengthen gut barrier function of epithelial cells in vitro in the absence of probiotic bacteria.11
Respiratory Barrier
The respiratory barrier provides protection against external particles by way of cilia and mucus. From the nasal cavity to the conducting bronchioles, the respiratory epithelium consists of ciliated pseudostratified columnar cells. The respiratory bronchioles and alveoli consist of simple squamous epithelial cells and are responsible for gas exchange as well as surfactant production.12 Airway epithelial cells serve a crucial role in preventing entry of irritants to areas where gas exchange is occurring. Numerous studies have shown that respiratory epithelia is compromised in patients with asthma. Respiratory epithelia dysfunction can lead to an aberrant immune response which in turn leads to inflammation and exacerbation of allergens.12 CpG-DNA, recognized by Toll-like receptor 9, has been shown to enhance the epithelial barrier integrity of healthy bronchial epithelial cells by increased tight junction molecule expression.13
Barriers Under Attack
Epithelial barrier damage is the common denominator of disruption to the skin, gut, and respiratory systems. This commonality is seen across a broad range of conditions from atopic dermatitis to inflammatory bowel syndrome to asthma. Akdis discusses how the link between skin barrier disruption and broad disease states can be used to prevent disease. Early protection of the epithelial barrier may have beneficial effects on the prevention and development of allergen sensitization in the first few years of life. Many environmental agents have been identified as damaging agents for epithelial barrier function.1 Some of these damaging agents include, but are not limited to: detergents, emulsifiers, and diesel exhaust particles (Table 1). The vast majority of these substances stem from modern industrialization and urbanization.
| Substance | Evidence |
| Polystyrene microplastic | Polystyrene microplastics damage gut barrier (Mouse models) |
| Exhaust particles and particulate matter | Particulate matter affects the alveolar barrier, causes defects in nasal epithelial barrier, and may stimulate myeloid dendritic cells to induce TH17 cells in ex vivo experiments |
| Anionic surfactants and commercial detergents/detergent residue | Keratinocyte cultures show that anionic surfactants and commercial detergents decrease tight junction barrier integrity in human skin |
| Emulsifiers in processed food | Emulsifiers increased damage to the structure to the small intestine in vivo and the translocation of Escherichia coli across M- cells in vitro in hamster model |
Table 1: Selected Epithelial Barrier Damaging Agents (after Akdis CA. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat Rev Immunol. 2021;21(11):739–51.)
Summary
Diseases with vastly different clinical manifestations have been linked to disrupted epithelial barriers. Epithelial damage can happen in many anatomical locations and with the complexity of immune regulation, it is vital to understand the mechanisms that affect the integrity of the skin, gut, and respiratory barriers. We believe the “epithelial barrier hypothesis” provides this critical understanding. This understanding allows for clinicians and researchers to develop preventative measures and therapies to restore epithelial barrier structure and function. Development of epithelial-protective agents can strengthen the skin, gut, and respiratory epithelia and in turn reduce the incidence and severity of inflammatory and autoimmune conditions. It is also crucial that as a society we limit our exposure to known epithelial barrier disrupters such as food emulsifiers, cigarette smoke, microplastics, etc. This is critical in preventing allergen sensitization. Continued research into epithelial barrier dysfunction is still necessary to develop strategies to reduce diseases associated with disrupted epithelial barriers. Biomarkers for leaky barriers, novel therapies for strengthening epithelial barrier molecules, blockage of bacteria and pathogenic colonization are a few possible therapies to further explore.

Krishna Patel, BS, is a first-year medical student at Kansas City University in Kansas City, MO.

Peter Lio, MD
Peter A. Lio, MD is a Clinical Assistant Professor of Dermatology and Pediatrics at Northwestern University Feinberg School of Medicine and a partner at Medical Dermatology Associates of Chicago.
References
- Akdis CA. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat Rev Immunol. 2021;21(11):739–51.
- Yazici, D., Ogulur, I., Kucukkase, O. et al. Epithelial barrier hypothesis and the development of allergic and autoimmune diseases. Allergo J Int 31, 91–102 (2022).
- De Benedetto A, Rafaels NM, McGirt LY, et al. Tight junction defects in patients with atopic dermatitis. J Allergy Clin Immunol. 2011 Mar;127(3):773-86.e1-7. doi: 10.1016/j.jaci.2010.10.018. Epub 2010 Dec 15. PMID: 21163515; PMCID: PMC3049863.
-
Simpson EL, Chalmers JR, Hanifin JM, et al.Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014 Oct;134(4):818-23. doi: 10.1016/j.jaci.2014.08.005. PMID: 25282563; PMCID: PMC4180007.
-
Horimukai K, Morita K, Narita M, et al Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol. 2014 Oct;134(4):824-830.e6. doi: 10.1016/j.jaci.2014.07.060. PMID: 25282564
-
Lowe AJ, Su JC, Allen KJ, et al A randomized trial of a barrier lipid replacement strategy for the prevention of atopic dermatitis and allergic sensitization: the PEBBLES pilot study. Br J Dermatol. 2018 Jan;178(1):e19-e21. doi: 10.1111/bjd.15747. Epub 2017 Dec 1. PMID: 28639306.
-
Groschwitz KR, Hogan SP. Intestinal barrier function: molecular regulation and disease pathogenesis. J Allergy Clin Immunol. 2009 Jul;124(1):3-20; quiz 21-2. doi: 10.1016/j.jaci.2009.05.038. PMID: 19560575; PMCID: PMC4266989.
- Kim JW, Kwok SK, Choe JY, Park SH. Recent Advances in Our Understanding of the Link between the Intestinal Microbiota and Systemic Lupus Erythematosus. Int J Mol Sci. 2019 Sep 30;20(19):4871. doi: 10.3390/ijms20194871. PMID: 31575045; PMCID: PMC6801612.
-
Tajik N, Frech M, Schulz O, et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat Commun. 2020 Apr 24;11(1):1995. doi: 10.1038/s41467-020-15831-7. PMID: 32332732; PMCID: PMC7181728.
- Rosenfeldt V, Benfeldt E, Valerius NH, Paerregaard A, Michaelsen KF. Effect of probiotics on gastrointestinal symptoms and small intestinal permeability in children with atopic dermatitis. J Pediatr. 2004 Nov;145(5):612-6. doi: 10.1016/j.jpeds.2004.06.068. PMID: 15520759.
- Abdelhamid L, Luo XM. Retinoic Acid, Leaky Gut, and Autoimmune Diseases. Nutrients. 2018 Aug 3;10(8):1016. doi: 10.3390/nu10081016. PMID: 30081517; PMCID: PMC6115935.
- Singh S, Dutta J, Ray A, et al. Airway Epithelium: A Neglected but Crucial Cell Type in Asthma Pathobiology. Diagnostics (Basel). 2023 Feb 20;13(4):808
-
Kubo T, Wawrzyniak P, Morita H, et al. CpG-DNA enhances the tight junction integrity of the bronchial epithelial cell barrier. J Allergy Clin Immunol. 2015 Nov;136(5):1413-6.e1-8. doi: 10.1016/j.jaci.2015.05.006. Epub 2015 Jun 19. PMID: 26100085.