Description: A 29-year-old man with psoriasis presents years after achieving good control with supposed “chigger bites” after a camping trip. Three months later, the itching bumps persisted and included scrotal and peripheral nodules. What’s your diagnosis?
Psoriasis, Insect Bites, and Prurigo Nodularis… or Is It?
By F. Hall Reynolds, MD
Dermatologist practicing in Chattanooga, Tennessee
CASE HISTORY
A 29-year-old man was known to have psoriasis for many years when he presented for alternate treatment to achieve better control. Typical psoriatic plaques were present over 45% of his skin surface, along with nail pitting and onycholysis. There was no evidence of psoriatic arthritis. The diagnosis was not in dispute.
After discussing various treatment options, the patient preferred topical steroids along with periodic exposure to commercial tanning beds since his travel as a symphony musician precluded proposed use of in-office narrow band UVB therapy.
However, he returned two years later with plaques covering 80% of his skin surface. At this point, he agreed to systemic therapy, choosing apremilast (Otezla, Amgen), which proved to be inadequate. Adalimumab (Humira, Abbvie) was then started at standard dosage, with near total skin and nail clearance.
After three years of good control, he noticed itching “chigger bites” after a camping trip. Three months later, the itching bumps persisted and included scrotal and peripheral nodules. Mineral prep was negative for Sarcoptes scabiei. Nonetheless, he was treated as a therapeutic trial with permethrin cream without improvement.


Biopsies for routine processing and immunofluorescence were obtained, along with tissue cultures. He was treated with ivermectin, hydroxyzine, and clobetasol while studies were pending; however, this regimen did not provide satisfactory results.
What is your diagnosis?
DISCUSSION
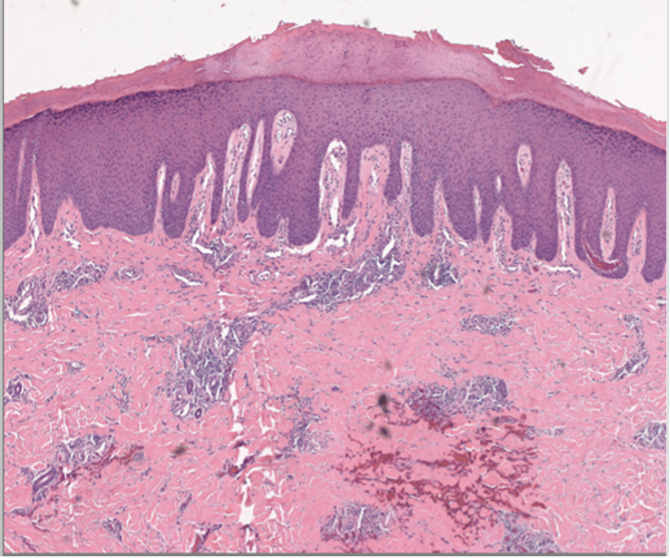
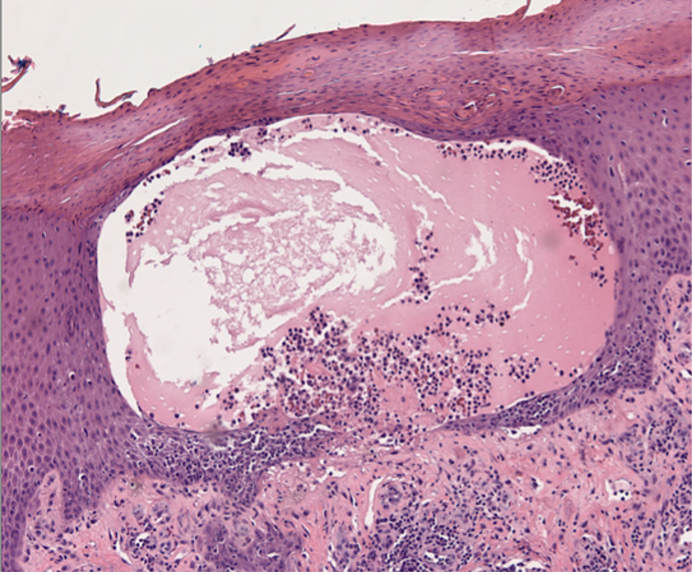
Tissue hematoxylin-eosin studies revealed findings typical of pustular psoriasis (Figures 3 and 4) with a negative direct immunofluorescence. Tissue culture was positive for heavy growth of Staphylococcus aureus.
A brief course of doxycycline and a change of psoriatic therapy to secukinumab (Cosentyx, Novartis) resulted in marked clearance of his skin. He was later changed to risankinumab (Skyrizi, Abbvie), which led to additional skin clearance.
Although the FDA recently approved spesolimab (Spevigo, Boehringer Ingelheim) for the specific therapy of generalized pustular psoriasis (GPP), there are instances where other biologics have been used successfully. In this case, secukinumab was chosen based on literature precedent.1
This case draws attention to two additional points. First, pustular psoriasis may well mimic arthropod assault clinically. Second, pustular psoriasis may eventuate into prurigo nodularis type lesions.2
REFERENCES:
1. Yeung J, Valbuena V. Successful use of secukinumab in pustular psoriasis. JAAD Case Rep. 2016 Dec 5;2(6):470-472. doi: 10.1016/j.jdcr.2016.05.006. PMID: 27981221; PMCID: PMC5148766.
2. Orozco Anahuati AP, Cardona Hernández MA, Navarrete Franco G, et al. Prurigo nodularis in a patient with pustular psoriasis, treated with tumor necrosis factor inhibitors. J Am Acad Dermatol. 2015; 72(5, suppl 1): AB245. doi https://doi.org/10.1016/j.jaad.2015.02.979


