A 45-year-old Caucasian female with a history of chronic eczema presents with red, pruritic eczematous patches with xerotic scale on the hands, feet, elbows, knees, and ankles, refractory to treatment. What is your diagnosis?
Eczematous Patches With Xerotic Scale
By Melissa Cheng, BS,1 Cynthia Lazzaro, DO,2 Samir Patel, MD3
1Western University of Health Sciences, College of Osteopathic Medicine of the Pacific, Pomona, California; 2Pacific Dermatology Specialists, Torrance, California; 3The Dermatology Group, Cincinnati, Ohio
CASE HISTORY
A 45-year-old Caucasian female presents to the dermatology clinic with red, pruritic, eczematous patches with xerotic scale on the hands, feet, elbows, knees, and ankles (Figures 1 and 2).
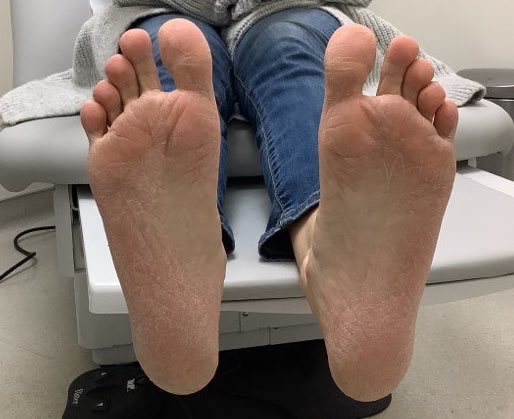

She has a history of chronic eczema on the hands for many years. Over the next 6 months, the patient was treated for suspected atopic dermatitis or tinea manuum and tinea pedis. During this time, she trialed treatments of clobetasol 0.05% topical ointment, econazole 1% topical cream, ketoconazole 2% topical cream, oral fluconazole, and ammonium lactate 12% lotion and showed no improvement of symptoms.
A 3-mm punch biopsy was performed since her skin was unresponsive to treatment. The biopsy showed hyperkeratosis, parakeratosis, acanthosis, and superficial lymphohistiocytic infiltrate (Figure 3a).
Deeper sections had alternating hyperkeratosis and parakeratosis, psoriasiform epidermal hyperplasia, and a focal suggestion of follicular plugging (Figure 3b).
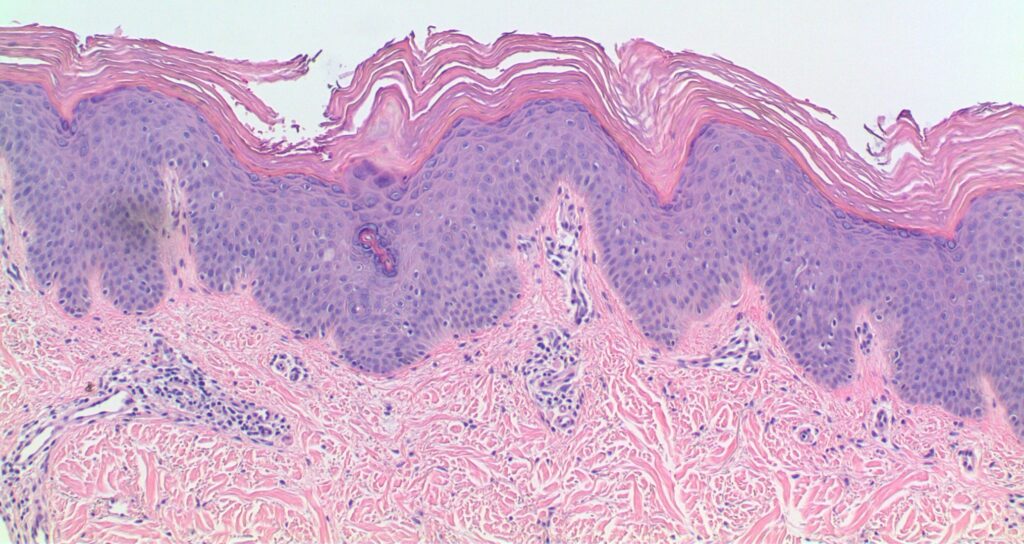
Figure 3. A) Hyperkeratosis, parakeratosis, acanthosis, and a superficial lymphohistiocytic infiltrate.
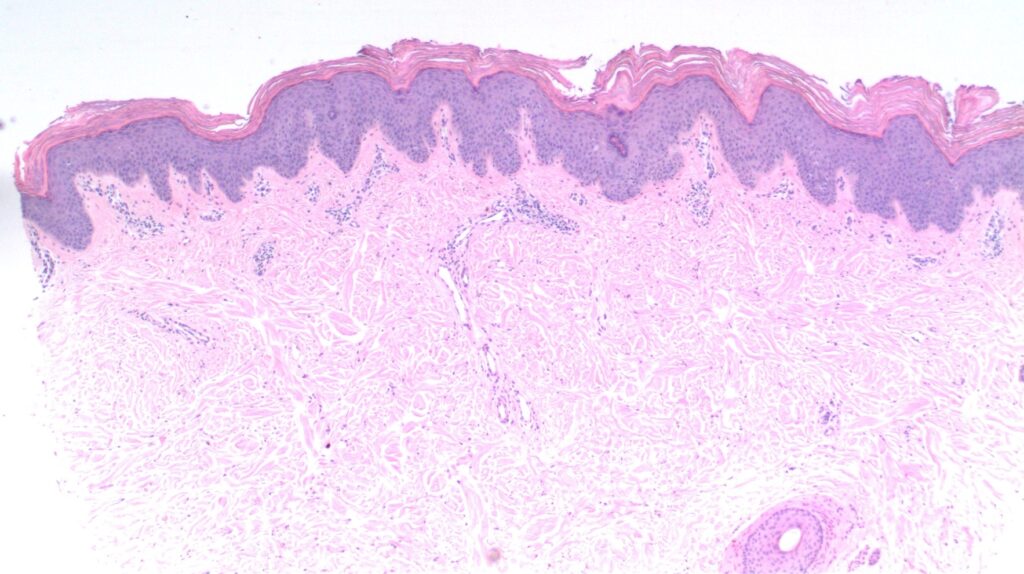
Figure 3. B) Deeper sections with alternating hyperkeratosis, parakeratosis, psoriasiform epidermal hyperplasia, and follicular plugging.
What is your diagnosis?
These results are suggestive of pityriasis rubra pilaris. Based on the clinical features of this patient’s presentation and histological findings she has type II subtype atypical adult pityriasis rubra pilaris (PRP).
DISCUSSION
PRP is a rare inflammatory disorder with unknown etiology. Its primary features are follicular hyperkeratotic papules and palmoplantar keratoderma, but it has a range of additional clinical presentations.
There are five subtypes of PRP based on Griffiths’ classification.1 A sixth subtype of PRP occurs in patients affected by HIV infection.
Classification of subtype is based on age of onset, clinical course, and morphologic features. Type I is classic adult. It is the most common adult subgroup and has acute presentation. Type II is atypical adult, a rare form that is chronic in nature.2 Atypical adult type II PRP is a rare subgroup that typically affects 5% of PRP patients and is chronic in nature, running a course of more than 20 years. Unlike type I PRP, type II does not follow the cephalocaudal progression. It is characterized by icthyosiform dermatitis, palmoplantar hyperkeratosis with lamellated scales, and hair sparseness or alopecia.3
We suspect that this patient has type II PRP because of the chronic nature of her symptoms and the morphological features of her disease.
There is no standardized treatment for PRP due to its rarity. Recommended treatments are based on patient presentation and disease severity. Treatments include topical corticosteroids, oral retinoids, methotrexate, biologics, and phototherapy. Most retrospective studies in the literature are looking at treatment of type I or the juvenile types of PRP, thus data is limited on the treatment of the type II subtype.
Topical corticosteroids showed most favorable outcomes in pediatric patients and those with type IV PRP in retrospective studies.3 Retinoids are the first-line systemic treatment for PRP. Isotretinoin was shown to have a 60% remission rate in type I PRP.4 There is a case of successful treatment of type II PRP with oral alitretinoin.5 Methotrexate demonstrated a 39% response rate in type I PRP.1 Biologics have been used for treatment-resistant PRP with favorable results, especially in the treatment of type II PRP. There are cases of successful use of secukinumab, etanercept, and ustekinumab for treatment of type II PRP.6-8 Additionally, there is a case of high-dose human intravenous immunoglobulin injections that was used successfully in the treatment of type II PRP.9
Treatment of PRP is challenging due to lack of good evidence and no standardized treatment. Our patient is continuing treatment with topical ammonium lactate 12% lotion and follow up is pending. The key point is to obtain biopsy in cases where skin is refractory to treatment. This patient was initially diagnosed with atopic dermatitis and tinea manuum and pedis. In cases of type II PRP where there is no standardized treatment, close follow-up is necessary, as the condition can persist for months or even years despite treatment.
REFERENCES
1. Griffiths WA. Pityriasis rubra pilaris. Clin Exp Dermatol. 1980;5(1):105-112. doi:10.1111/j.1365-2230.1980.tb01676.x.
2. Klein A, Landthaler M, Karrer S. Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol. 2010;11(3):157-170. doi:10.2165/11530070-000000000-00000.
3. Wang D, Chong VC, Chong WS, Oon HH. A Review on Pityriasis Rubra Pilaris. Am J Clin Dermatol. 2018;19(3):377-390. doi:10.1007/s40257-017-0338-1.
4. Borok M, Lowe NJ. Pityriasis rubra pilaris. Further observations of systemic retinoid therapy. J Am Acad Dermatol. 1990;22(5 Pt 1):792-795.
5. Pampín A, Gómez-de la Fuente E, Caro Gutiérrez MD, López-Estebaranz JL. Successful treatment of atypical adult pityriasis rubra pilaris with oral alitretinoin. J Am Acad Dermatol. 2013;69(2):e105-e106. doi:10.1016/j.jaad.2013.01.036.
6. Gauci ML, Jachiet M, Gottlieb J, et al. Successful treatment of type II pityriasis rubra pilaris with secukinumab. JAAD Case Rep. 2016;2(6):462-464. Published 2016 Dec 5. doi:10.1016/j.jdcr.2016.09.006.
7. Kim JH, Park MC, Kim SC. Etanercept-induced clinical remission of type II pityriasis rubra pilaris with rheumatoid arthritis. Acta Derm Venereol. 2012;92(4):399-400. doi:10.2340/00015555-1367.
8. Napolitano M, Lembo L, Fania L, Abeni D, Didona D, Didona B. Ustekinumab treatment of pityriasis rubra pilaris: A report of five cases. J Dermatol. 2018;45(2):202-206. doi:10.1111/1346-8138.14114.
9. Kerr AC, Ferguson J. Type II adult-onset pityriasis rubra pilaris successfully treated with intravenous immunoglobulin. Br J Dermatol. 2007;156(5):1055-1056. doi:10.1111/j.1365-2133.2007.07773.x.

