Belly fat is more strongly linked to psoriasis risk than total body fat, particularly in women, a new study shows.
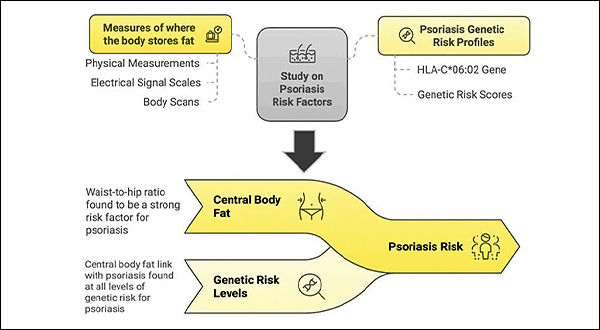
This link remained consistent regardless of genetic predisposition, indicating that abdominal fat is an independent risk factor for psoriasis, according to the research which appears in the Journal of Investigative Dermatology.
For the study, researchers analyzed data from over 330,000 participants with White British ancestry in the UK Biobank, including more than 9,000 people with psoriasis. They examined 25 different measures of body fat using both traditional methods and advanced imaging techniques, assessing how each was associated with psoriasis.
Where Fat is Stored Matters
“Our research shows that where fat is stored in the body matters when it comes to psoriasis risk. Central fat — especially around the waist — seems to play a key role,” says Lead Investigator Ravi Ramessur, MD, St John’s Institute of Dermatology, King’s College London, in a news release.
“This has important implications for how we identify individuals who may be more likely to develop psoriasis or experience more severe disease, and how we approach prevention and treatment strategies.”
Catherine H. Smith, MD, also at St John’s Institute of Dermatology, King’s College London, and senior author adds, “As rates of obesity continue to rise globally, understanding how different patterns of body fat influence chronic inflammatory conditions such as psoriasis is important. Our findings suggest that central body fat contributes to psoriasis risk irrespective of genetic predisposition and reinforces the importance of measuring waist circumference and proactive healthy weight strategies in psoriasis care.”
Because this study only included individuals of White British ancestry from the UK Biobank, the generalizability of these findings to more diverse populations may be limited. Future studies incorporating datasets with dermatologist-confirmed diagnoses and broader ethnic representation will be important to further validate these associations and refine risk stratification approaches, the study authors conclude.
Dr. Ramessur notes, “We were surprised by how consistently strong the association was across different central fat measures and how much stronger the effect was in women. The observed links between central body fat and psoriasis suggest that there may be underlying biological mechanisms contributing to the disease that are not yet fully understood and which warrant further investigation.”
In an accompanying editorial, Joel M. Gelfand, MD, MSCE, FAAD, of the Department of Dermatology and Center for Clinical Sciences in Dermatology, University of Pennsylvania Perelman School of Medicine in Philadelphia, PA, points to the potential of incretin therapy for psoriatic disease. Incretins are gut-derived hormones, principally glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP), that regulate glucose, digestion, and appetite, and are approved for treatment of diabetes, obesity, and obesity-associated obstructive sleep apnea.
“The strong relationship between psoriasis and obesity and the emerging promise of glucagon-like peptide-1 receptor agonists (GLP1RA) for reducing psoriasis morbidity is a call to action for large-scale clinical trials of GLP1RA monotherapy for treatment of psoriasis,” writes Dr. Gelfand. “Our current paradigm of just focusing on the skin and joint manifestations when treating psoriasis is outdated in the context of our evolving understanding of the tight relationship of psoriasis, obesity, and cardiometabolic disease.“