Janus kinase (JAK) inhibitors are revolutionizing the way certain inflammatory diseases such as atopic dermatitis (AD) are being treated, but a more nuanced approach may be needed in modulating JAK activity for conditions like asthma.
This is the main takeaway message from a new study in the December 21, 2023, issue of Cell.
For the study, researchers used a mouse with a patient-specific mutation in the gene for JAK1 to show how this mutant protein causes disease and could be harnessed for broader therapeutic use. They found that JAK1 signaling has varying or even opposing effects in different cell types and tissues, including an unexpected immunoregulatory role in lung sensory neurons, where it suppresses lung inflammation.
“Safety aside, the JAK inhibitors are the most effective medications to date for AD, and more specifically JAK 1 selective inhibitors are particularly exquisite,“ says Brian Kim, MD, MTR, FAAD, the Sol and Clara Kest Professor of Dermatology, Vice Chair for Research, and Director of the Mark Lebwohl Center for Neuroinflammation and Sensation at Icahn Mount Sinai in New York City, tells TDD.
Some people are born with a type of JAK1 gain-of-function (GOF) mutation. This was first reported by study co-author Stuart Turvey, MBBS, DPHIL, FRCPC in 2017 in patients with an immune dysregulatory and hypereosinophilic syndrome characterized by severe eczema and asthma. A JAK1 GOF mutation makes JAK1 more active than normal, leading to overactive immune responses and may cause health problems like autoimmune diseases or cancer.
“If you simply have a mutation to JAK1, you are predisposed to develop AD, and AD patients with this mutation respond to JAK1 inhibitors, but so do patients with run-of-the-mill AD,” Dr. Kim says.
There could be other mutations, variants, or some other modifiers at play, he says.
Growing numbers of people with the JAK1 GOF mutation and others along the STAT6 pathway, which is downstream of the JAK1 pathway, are being identified. “We are learning from mutations in rare conditions about general disease,” he says.
Digging Deeper
The guiding thought was that if you activated JAK1, you would get inflammation throughout the body, but this may not be the case.
“The new study showed that JAK1 activation in nerves of the lung is actually protective,” he tells TDD. “In the skin, JAK produces itch, but in the airway, it activates nerves to turn inflammation off.”
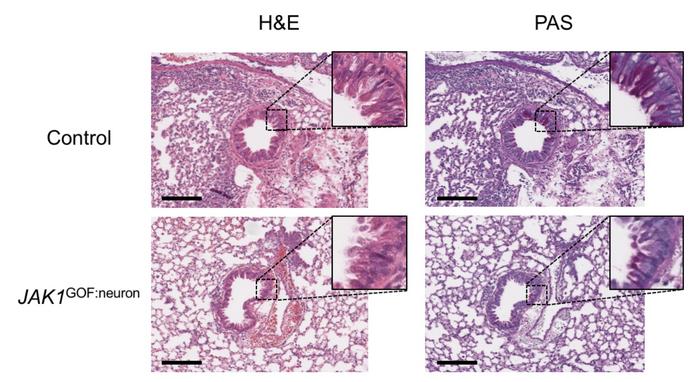
In the lung neurons of the mice, the JAK1 mutant protein reduced inflammation caused by exposure to mold by producing substances that suppress inflammation. However, the mice still showed the same skin condition as the original patients that Dr. Turvey reported on in 2017, indicating that JAK1 signaling has different effects in different cells and even within the same cell type in different parts of the body.
Research on several inhaled JAK inhibitors for asthma was stopped early possibly for these reasons, Dr. Kim speculates.
“AD is not a skin version of asthma,” he says. “They are all different diseases even though they are in the same family.”
Now, the researchers plan to examine how additional genes along the JAK pathway may also inform tissue-specific patterns of disease.